Orthopaedic Expert Care You Can Trust

What is it?
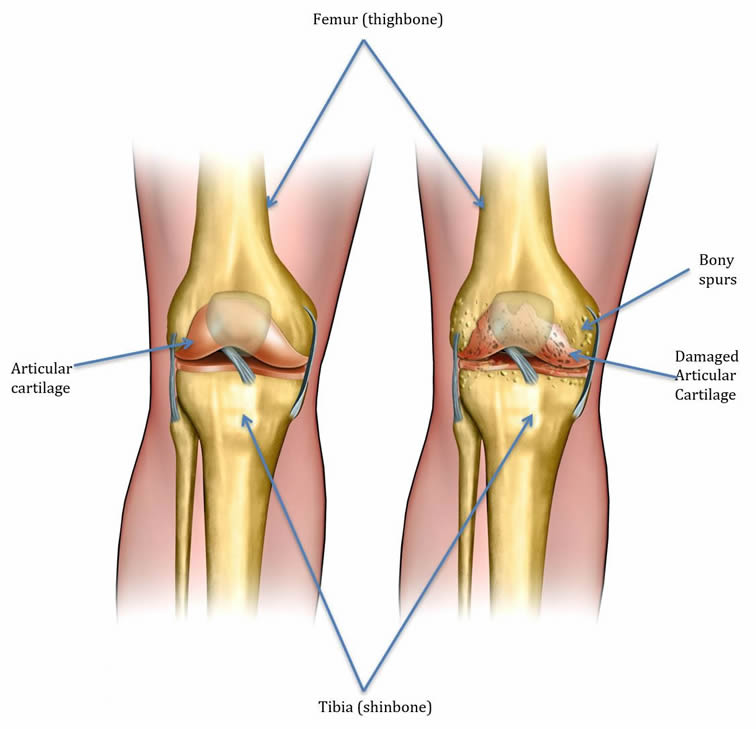
The knee joint is a hinge joint, formed by end of the femur (thigh bone) and the top of the tibia (shin bone). This is very smooth and allows friction free movement. This smooth movement is further facilitated by synovial fluid in the joint. In the initial stages of arthritis, the cartilage becomes soft and loses water content. This progresses to thinning of cartilage and ultimately small areas of cartilage are completely gone from the ball and socket such that bone is in contact with bone. This is effectively end-stage arthritis. The knee is made of three compartments:
- Medial (inside aspect of the knee)
- Lateral (outside aspect of the knee)
- Patello-femoral (behind the knee cap)
As we get older, the quality of the cartilage and its properties degrade with time and some wear and tear is normal. Arthritis however can also occur after a specific injury/trauma, or from inflammatory diseases such as rheumatoid arthritis and psoriatic arthritis. The most common type of arthritis in the UK is osteoarthritis (OA), which is non-inflammatory and normally occurs because of wear and tear.
What are the symptoms?
The symptoms and knee arthritis do not always correlate with the x-ray findings and the degree of cartilage loss. If you have any of the symptoms below that are affecting your activities of daily living, it is important to see your doctor for further evaluation. The main symptoms are pain and stiffness, though patients may also have feelings of crunching sensation and the knee giving way. Symptoms can be worse in the morning or after period of rest.
Pain
The location of pain can be variable, and largely depends on which compartment is most affected by the arthritis (e.g. predominantly medial compartment arthritis is likely to lead to pain mainly on the inside of the knee). If there is significant arthritis behind the kneecap, then pain is felt in front of the knee and is worse on stair climbing and walking downhill.
Stiffness
This can occur after prolonged sitting or after period of rest. Patients with inflammatory arthritis have morning stiffness of greater than 30 minutes.
Patients also complain about difficulty bending over or kneeling, touching toes, and putting shoes and socks on.
How is knee arthritis diagnosed?
In the vast majority of cases, I can make the diagnosis by simply taking a detailed history and performing a thorough examination. X-rays are usually done on the same day and treatment options discussed after the x-rays performed. X-rays also allow the surgeon to plan surgery if required.
I like to perform special types of x-rays using calibration sphere. This allows me to meticulously plan any future surgery using templating software. Therefore, even if you have had x-rays in the past I may ask for x-rays to be repeated in order to facilitate this planning step. It is rare to require a MRI scan to diagnose knee arthritis.
What are the treatment options available?
In the early stages of arthritis, simple measures such as modifying your activity, resting, and anti-inflammatory medications can help significantly relieve pain. Weight loss can also help considerably. When these measures have failed, your GP or physiotherapist may refer you to an orthopaedic consultant. You can rest assured I will use all possible joint-preserving techniques if possible before talking about a total knee replacement. This includes joint injections, using knee braces to unload one of the affected compartments and physiotherapy with an aim to maintaining muscle bulk and increasing strength. However, ultimately, the only permanent surgical resolution to pain from arthritis is a total knee replacement.
If you’re suffering from pain and stiffness in your knee joint, the first step to feeling better is to schedule an appointment with Mr Parag K Jaiswal, an expert in hip and knee problems. I will be happy to discuss all treatment options, especially ones that can save your joint. To request an appointment call 0207-459-4882