Orthopaedic Expert Care You Can Trust

Total hip replacement is one of the most successful operations known. In the vast majority of cases it enables people to live a more active life with significantly less pain. However, it is an artificial joint and will wear out with time and fail. This can occur over a variable period of time. We can say with some certainty approximately 90 to 95% of hip replacement last over 10 years.
In revision hip surgery, a variety of different surgical techniques can be used, varying in the complexity and length of surgical time. For example in some cases only the liner of the socket needs to be replaced whilst at the other end of the spectrum both components (the socket and the stem) need to be removed. Upon removal there may be missing bone requiring substitution with a bone graft from a donor, or the use of metal implants and augments to restore the hip joint to where it should be.
Why would you need a revision total hip replacement?
Loosening and implants wearing out
In order for a hip replacement to function well the implants on both sides (the socket and the stem) must remain firmly attached to the bone. At the time of the initial operation the components were either firmly adhered to the socket or the thigh bone (femur) with cement or with out. The cause of the loosening is not always obvious. Usually, repetitive high impact activities, excessive bodyweight (body mass index), and wearing away of the plastic liner between the ball and socket are all contributing factors. Younger patients typically use the hip joint more and therefore are likely to need revision surgery in the future.
Infection
Infection is a potential complication of any surgery. If it does occur following a hip replacement it can be superficial or deep. Deep infection occurs when the bacteria attach to the surface of the implants or artificial joint. Infection can occur early (within the first 30 days of an operation) or late, many years after an operation. The infection process can lead to loosening of one or both components of a hip replacement. There can be issues with wound healing too with the development of persistent discharge.
There are different ways that infection can be managed and a number of factors need to be considered when approaching how to deal with this difficult problem. A multidisciplinary team (MDT) comprising of microbiologist, radiologist, physiotherapist, and other surgeons are used to tackle this problem and to determine the best way to deal with this. This wil be discussed in detail with you if this is the cause for the revision surgery. I work with some leading microbiologists and radiologists in the field and we hold weekly MDTs to discuss difficut cases.
Dislocation
In a hip replacement, the artificial ball is smaller than your native hip. For a hip replacement to work well the ball must remain inside the socket for the entire functional range of movement the individual has. The position of instability depends on how the hip joint is approached during the initial operation. The greatest risk of dislocation after the first operation is usually the first 12 weeks. As the hip gets worn out, there is a higher incidence of late dislocation further on down the line (10 or more years). If you experience recurrent dislocation especially more than three times in a short period of time, then you may need to have revision surgery. This will involve removing one or both components of your hip replacement and putting in more specialised implants that lower the risk of dislocation.
Fracture
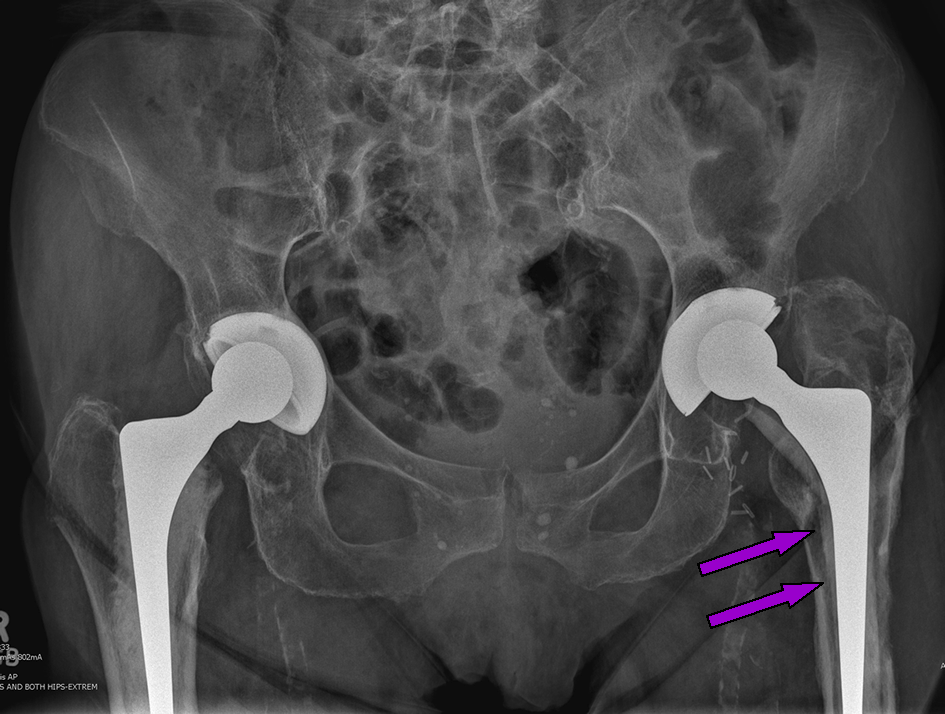
When the thigh bone breaks around the stem of the hip replacement, it is called a periprosthetic fracture. This can typically occur with a fall from a standing height in frail bone, or trauma with high energy (e.g. a road traffic accident). Not all periprosthetic fracture require revision surgery (the stem to be taken out and the new one put in). Sometimes these fractures can be fixed with plates and screws and the old implant retained.
In the case on the right the broken thigh bone (femur) has been fixed so well that the fracture line cannot be seen. The femur is held with plates and screws around the implant. This 90 year old lady was then walking with all her weight on her leg the next day.
Reaction to metal ions and metal allergy
Metal on metal hip replacements have been implanted in the past and you may have heard about them in the media. This is when both the socket and the ball of the artificial joint are made of metal. This can generate metal ions locally around the hip joint, which then causes an inflammatory reaction leading to loosening and local destruction of tissue such as muscle and bone around the hip. Very rarely, patients can be allergic to some types of metal used in implants. This can cause pain. There is no definite consensus among orthopaedic experts regarding this; further research into this area needs to be conducted.
What if you need a revision total hip replacement?
The prospect of having revision surgery can be very daunting for you. Rest assured, I will perform a thorough medical evaluation to determine your fitness for surgery. A number of tests will be performed to ensure we have the right diagnosis and meticulously plan the surgery.
Your mobility will often be temporarily limited after surgery. Depending on the surgery performed, crutches will be required usually for a period of 6 weeks and sometimes 12 weeks. Therefore you may need help with tasks of daily living, such as cooking, shopping, and bathing.

Why choose Mr. Jaiswal?
As result of my dual fellowship training and extensive Consultant experience in a tertiary hospital (where other orthopaedic consultants refer patients with complex problems), I perform, revision surgery regularly, using cutting edge surgical techniques and the latest, innovative prosthesis. I have an excellent team which help me achieve the best possible results. We regularly discuss cases in a weekly MDT with other consultants to ensure we have a consensus on how best to treat these often very challenging problems. I closely monitor the results of all my cases, and to date, every revision procedure I have performed has been successful.