Orthopaedic Expert Care You Can Trust

What does the operation involve?
You are usually admitted on the day of surgery and the hospital will contact you regarding the ideal time for you to come in. The operation can be performed under spinal anaesthesia with sedation or a general anaesthetic. You are not allowed to have any food six hours before your surgery but you can drink clear fluids (water only) up to 2 hours before your surgery time.
A tourniquet (like a blood pressure cuff on the arm) is placed on your thigh above the knee. This restricts the amount of bleeding that occurs during the operation. The scar is made along the middle of your knee. As mentioned previously the knee joint is reshaped to take the components, which are fixed onto the bone with the use of cement (this acts as grout). All the structures that were cut are then repaired (e.g tendons). A waterproof dressing is applied and the whole knee is covered with a bulky bandage. The bandage gets taken off the next day.
What happens after the operation?
If you’ve had a general anaesthetic, you usually wake up in the recovery area after the operation. I prefer my patients to have a spinal anaesthetic
– then they can see me lifting their leg and seeing how straight it is! It is also part of the enhanced recovery programme is use.
Do you not be too alarmed to see a drip line in your vein when you wake up. This is normal and fluids are given through this. Patients that have had spinal anaesthesia usually have good pain relief for the rest of the day. I use enhanced recovery protocols, so that my patients are usually walking on the day of surgery (with the help of physiotherapist). The knee can become very painful that night or certainly the next morning and you will be written up for strong painkillers that I give to all my patients regularly. Always ask the nurses on the ward if you are still in pain.
Post-operative Physical Activities
It is imperative that you keep the knee moving after the operation. The first three days can be very painful. The physiotherapist will begin teaching you how to move your knee and how to walk with crutches. You will be allowed to put all your weight on the knee and most patients end up leaving the hospital using crutches. They usually stay in hospital for 3 to 4 days. Due to the enhanced recovery program I use, and relatively short tourniquet times, I encourage my patients to walk on the same day of surgery and this has been shown to lower the length of stay in hospital with patients having less pain.
General advice
As mentioned previously, patients are often in a lot of pain in the first three days, which can continue for two weeks. It is important to ask for painkillers and ensure you take them regularly. Obviously, everyone is different and the degree of pain experienced can vary widely. Consistently, there is always swelling and bruising which can continue for 2 to 3 months. Occasionally, it can go on for six months. The stitches or clips are usually removed by the nurse at your GP practice around two weeks after the operation. Until then the wound needs to be kept dry with a waterproof dressing on at all times.
It’s very tempting to place a pillow under your knee when in bed or resting on the sofa, as patients often find this is a comfortable position. Please try and resist this, as there is a danger that the knee gets stuck in that position and cannot be straightened fully. Take care not to stay in one position whilst in bed. Moving every hour can help prevent getting sores on the back of your heels and buttocks.
Most surgeons review their patient six weeks after the operation. You should try and increase your physical activity each day during this six-week period. It is also important to keep exercising your knee and making sure that the movement is maintained.
When can I drive and how long do I need to take off work?
Most people return to driving around the six week mark. Once again, due to the enhanced recovery program and minimally invasive techniques I use, I advise my patients to return to driving as soon as they can do an emergency stop. This can be around 3 to 4 weeks following surgery.
Return to work is that little more difficult to answer. This largely depends on the nature of your work. Often return to work correlates with when the patients can drive. Most patients take a minimum of six weeks off.
What are the risks of the operation?
All surgery carries risks. The main risks regarding this particular operation include:
Infection
This may be superficial or deep. Antibiotics are usually used to treat superficial infections. Deep infections may require further surgery to eradicate the infection. A deep infection can be a life-changing event, but fortunately are a rare occurrence.
I regularly consult with my microbiologist to give the best possible antibiotics to prevent this complication from occurring. Keeping the surgical time to a minimum also helps prevent infection. I perform the surgery in a special laminar flow (ultra clean) operating theatre to further lower the risk of infection.
Blood clots
A blood clot in the leg is called a deep vein thrombosis (DVT). This can occur in either leg following surgery. A pulmonary embolism (PE) is when the clot migrates to the lungs. This is less common than a DVT but very rarely, can be fatal.
You will be given blood-thinning medications to lower the risk of getting clots. The sooner you are walking and more active, the lower the risk of getting blood clots. Again, this is why I use enhanced recovery programs to enable my patients to be up and walking early.
It is advisable to not go on any long distance flights for at least six weeks, but it is better still if you delay for 12 weeks.
Nerve injury
Numbness on the outer aspect of the scar is quite common. It’s not a cause of pain, but rather patients are aware of an altered sensation. Very rarely, the nerve that supplies muscles to the ankle and foot (common peroneal nerve) may get compressed or damaged leading to a foot drop.
Instability
The knee might feel wobbly after the operation. This could be due to a number of reasons and will need a thorough clinical assessment with x-rays. You may well need an examination under anaesthesia to determine the cause of the instability.
Stiffness and ongoing pain and swelling
It is imperative that you do exercises at home to regain the movement you had in your knee before the surgery or to improve it afterwards. The physiotherapist usually give you a program to do. Nonetheless, stiffness in the knee can still occur. This is usually dealt with extensive physiotherapy. However, a manipulation under a general anaesthetic may be required to break down the scar tissue that has formed causing stiffness. If this is needed, then you are usually put in a continuous passive motion machine. This slowly and smoothly bends and straightens the knee to maintain the range of motion that was accomplished after the manipulation.
Dissatisfaction rate of 20%
All patients that have had a joint replacement surgery in the UK have the data entered in the National joint registry. This is the largest registry of its kind in the world and has approximately 3 million entries. From this data, we can conclusively say that a knee replacement is a successful operation 80% of the time. However, this means that there is still a dissatisfaction rate of around 20%. A lot of research is going into why this is the case and I have presented in several international meetings regarding this.
Loosening
All artificial joints have a finite lifespan and wear out with time. The National Joint Registry (NJR) has shown us that 90% of knee replacements last more than 15 years.
If you have any questions regarding this or any other hip or knee problems, give us a call. I will be very happy to help.
Why Choose Mr. Jaiswal?
As a result of completing two fellowships (2 years of highly specialised training in hip and knee surgery), I have extensive experience in performing simple and complex total knee replacements. If possible, I use minimally invasive techniques and always use enhanced recovery programs, thus resulting in better pain relief after the operation. Furthermore, patients are quicker to mobilise and have shorter length of stays in hospitals.
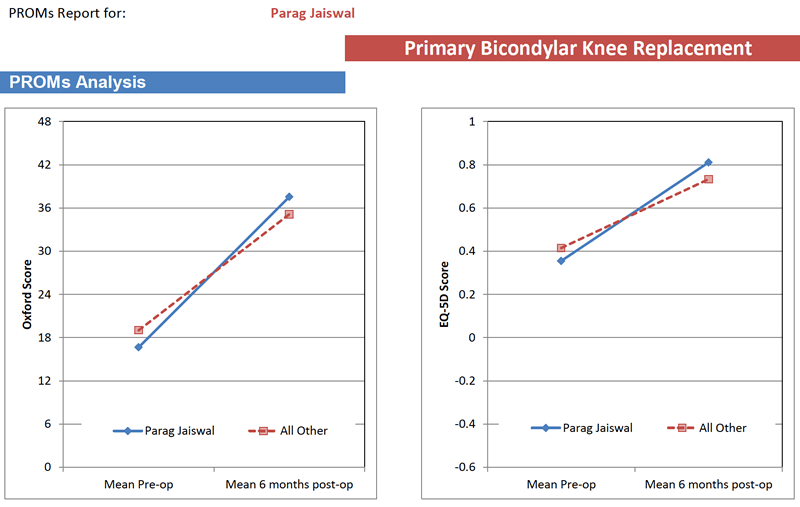
As I mentioned previously, all patients undergoing joint replacement surgery have their data entered in the National Joint Registry (NJR). All patients are requested to fill in a 12-point questionnaire assessing the pain and function in their hip (called the Oxford Knee Score) before and 6 months after surgery. The graph below shows that my patients (blue circle) have experienced greater gains than the national average (red dashed line) following a knee replacement and tend to do better.